The service is based at Endoscopic Treatment Unit, First Floor Corridor, Macclesfield District General Hospital, Victoria Road, Macclesfield, Cheshire, SK10 3BL.
Contact: 01625 661044 (ward) or the Booking Team: 01625 663333.
Macclesfield District General Hospital has a state-of-the-art endoscopy unit comprising five endoscopy rooms, two recovery areas and a self-contained decontamination unit.
It delivers the full range of diagnostic and therapeutic procedures which include ERCP, EMR, surveillance, colonoscopy, bowel cancer screening programme, PEG, and a bronchoscopy service.
Colon capsule endoscopy (CCE) and trans-nasal endoscopy (TNE) are supported by endoscopy but are carried out in our new Elective Treatment Centre.
Consultant Gastroenterologist(s)
Dr Konrad Koss
Dr Ramasamy Saravanan
Dr Daniela Radford
Dr Hatim Mudawi
Lower GI Surgical Consultants
Mr Usman Khan
Mr Kayode Habeeb
Mr Simon Ward
Mr Mohammed Sadat
Mr Mohamed Nizam
Mr Abubaker Elhaj
Mr Mario Metry
Nurse Endoscopists
Mark Morrison
Dignity Champion
Michelle Perry

Your Dignity Champion pledges to:
- Stand up and challenge disrespectful behaviours
- Act as a good role model by treating other people with respect, particularly those who are less able to stand up for themselves
- Speak up about dignity to improve the way that services are organised and delivered
- Influence and inform colleagues
- Listen to and understand the views and experiences of patients
What is a Gastroscopy?

A gastroscopy (or simple endoscopy) is a test which allows the endoscopist to look directly at the lining of the oesophagus (gullet), the stomach, and the first part of the small intestine (duodenum). In order to do this, a thin flexible tube called a gastro scope that transmits live video images to a TV monitor is passed through your mouth into your stomach.
Why am I having a Gastroscopy?
Your doctor wants to find out if there is a reason for the symptoms you are having. The endoscopist will get a clear internal view. Importantly, this is the only test that allows biopsies to be taken for analysis.
Are there any alternatives to the test?
Yes, a barium swallow or meal are x-ray test which will show larger abnormalities of the musoca (lining) but biopsies cannot be taken.
What are the risks?
A gastroscopy is a safe test – serious complications are uncommon. Occasionally the gastroscope can damage the lining of the oesophagus, stomach or intestine.
In order for you to be able to give informed consent, you should be aware of the risks of the procedure.
The clinician requesting the test will have considered these risks in relation to the benefit of having the procedure for diagnosis and/or treatment. The risks are associated with the procedure itself and with the administration of sedation.
● There is a risk of causing a tear (otherwise known as a perforation) in the gullet or stomach with the camera. This risk is very small and can occur in 1 in 2000 cases. Treatment would depend on the severity and would require admission to hospital, treatment with antibiotics and possible surgery to repair the hole.
● There is a risk of causing bleeding at the site of biopsies but this is uncommon, usually minor and usually stops on its own. Rarely, bleeding may necessitate a blood transfusion or further procedures to stop the bleeding.
● You may experience bloating and abdominal discomfort for a few hours after the procedure because air is used to inflate the stomach. This can often be relieved by belching.
● You may have a sore throat for 24-48 hours. Please tell the nurse if you have any loose teeth, caps or crowns as there is a risk that they can become dislodged during the procedure.
● Sedation can occasionally cause problems with breathing, heart rate and blood pressure. You will be monitored throughout the procedure, so that any potential problems can be identified and treated rapidly. If you have an existing heart or breathing condition, you will be assessed prior to the procedure.
Before admission:
Please remember no food for six hours before the test and clear fluids only until two hours before the test. This is very important as we cannot do the test if you have eaten.
What should I expect?
• On arrival, report to the reception desk in Endoscopy Unit. Your details will be checked and you will be asked to take a seat.
• A nurse will collect you and take a brief medical history from you, including a discussion of your current medication, discharge arrangements and the test itself.
Please inform the nurse of any allergies. Please ask questions if you have any.
• You may be asked to wait a short while until you have the test.
• A nurse or endoscopist will ask you to sign the consent form making sure you understand the test.
• You do not need to get undressed, but you will need to take off your coat.
• The ward is a single sex area*.
*East Cheshire NHS Trust is committed to equality and equity for all communities and to providing services which are accessible, appropriate and which recognise the diversity of people, their needs and choices.
To deliver a patient-led service, the Trust must ensure that services and care delivery recognise
the needs of each individual service user including transgender (trans) and gender diverse service users.
Is the procedure painful?
The test is not painful however you may experience some retching as the tube touches the back of your throat. You may feel bloated and burp because air is put into your stomach to ensure good views. The test usually lasts between five and 15 minutes.
These feelings are not pleasant but do not last long.
There are two ways you can have the test:
1. You can have local anaesthetic spray to the back of the throat which numbs the area and makes it easier to the pass the tube. It also reduces retching.
2. You can have a mild sedative which will help you feel more relaxed about the test. It does not put you to sleep.
If you do not wish to have any of these options, please inform the nurse.
During the test
- You will be taken into the procedure room. In the room will be the Endoscopist and two nurses who will stay with you during the test
- Your throat will be sprayed with local anaesthetic or you will be given the sedative injection if you have requested it.
- You will be made comfortable on your left side. A pad will be placed under your chin.
- A plastic mouth guard will be placed gently in your mouth.
- The endoscope will be passed across the top of your tongue to the back of your throat. Try to breathe steadily and remain calm.
- It will then be passed down the gullet, into the stomach and the small intestine.You may feel bloated as air is used to inflate your stomach to get good views.
- Biopsies can be taken and this is painless.
- Photographs may be taken of normal and abnormal mucosa.
- If you get a lot of saliva in your mouth, the nurse will clear it using a suction tube.
- The endoscope is removed slowly taking some air out at the same time.
- The mouth guard will be removed and a tissue provided to wipe your mouth.
- You will be made comfortable
- You will be taken out to the ward area to recover.
When can I go home?
If you have had local anaesthetic you can go home as soon as you feel well enough. You need to wait 30 minutes before having a drink to ensure the spray has worn off. If you had a sedative then we will only discharge you when you are safe to go home and you feel happy to do so. You will need to wait approximately an hour after the procedure before you eat or drink anything. You need to be collected from the unit by a responsible adult who will stay with you overnight.
If you have had sedation - FOR 24 HOURS, YOU MUST NOT:
- Drive
- Operate machinery
- Drink alcohol
- Sign legal documents
How will I feel afterwards?
- Your throat may feel sore but will settle without treatment.
- You may feel bloated because air remains in your stomach, again it will settle without treatment.
- You should be able to eat and drink as normal once the effects of the throat spray have worn off.
When will I know the results?
- If you have throat spray, you will be told what has been seen and done after the test.
- If you have been sedated, when you are fully awake, you will be told the information. If you would like a family member or friend to be present as you may forget what you have been told, please inform the nurses.
- You will be given a discharge leaflet which includes aftercare, useful telephone numbers and information about your test.
- The hospital consultant responsible for your procedure will receive any biopsy results and will write to you or see you in Outpatients. A copy of the report will also be sent to your GP.
The consent form
You will find a consent form with this information. This gives the endoscopist a formal indication that you are agreeing to undergo the procedure as described. You keep a portion of the form as your record.
Please read the consent form and bring it with you to the appointment.
For further information, click here.
What if I decide not to have the test?
If you read this information and decide not to go ahead with the test, please ring the Booking Centre, using the telephone number on your appointment letter, to let us know. You should also discuss your decision with your GP or hospital consultant.
Colonoscopy
Introduction
Your specialist has recommended that you have a colonoscopy to investigate your symptoms.
You will be asked to attend Macclesfield District General Hospital Endoscopy Unit.
Your appointment
- Please check your appointment letter before attending to make sure you attend the correct site.
- If you request sedation, you need to be collected from the unit by a responsible adult who will stay with you overnight.
- As you will need to see the nurse first, the time you are given to attend is not the time of your colonoscopy.
- The time is approximate due to different procedures taking different time periods.
- Emergency procedures may take priority.
- Expect to be in the unit for up to four hours approximately.
What if I decide not to have the test?
If you read this information and decided not to go ahead with the test, please let us know by calling the Booking Centre on 01625 663333. You should also discuss your decision with your GP or hospital consultant.
What is a colonoscopy?
A colonoscopy is a test which allows the doctor/nurse specialist (endoscopist) to look directly at the lining of your large bowel (colon).
A long flexible telescope (colonoscope), about the thickness of your index finger, with a bright light at its tip is carefully passed through the bottom (anus) to the caecum and the end of your small intestine.
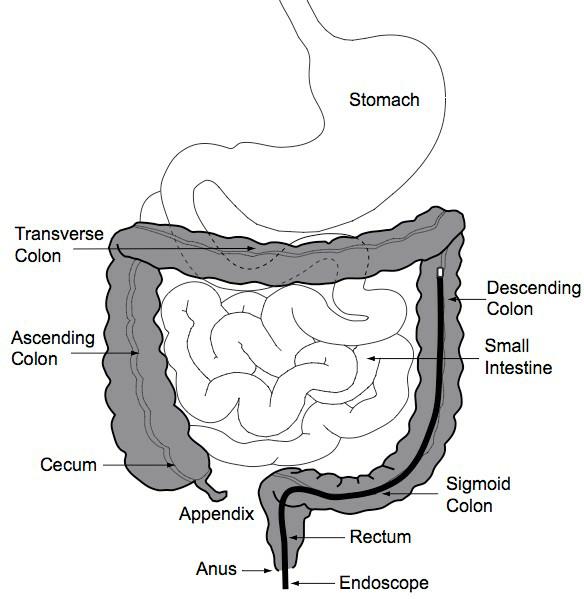

- A digital video camera on the colonoscope transmits pictures of the inside of your colon to a monitor. This enables the endoscopist to be able to look for any abnormalities.
- A biopsy (small piece of tissue) may be taken using tiny biopsy forceps. This does not cause any pain.
- If polyps (projections of tissue, rather like tiny mushrooms) are found, it is possible to remove them or a biopsy taken to be sent for further tests.
- Sometimes polyps can bleed.
What are the benefits and risks?
The procedure helps to investigate symptoms and be able to treat them.
A colonoscopy does have its risks but major and serious complications are rare. These risks will be discussed with you before you sign the consent form.
These can include:
- Minor bleeding. Slight spotting of blood on the toilet paper or small drops in the toilet bowl should be expected however, this should stop quickly within a few days.
- Significant bleed can happen if a polyp is removed, however the risk of this is less than one in 200. It is advisable not to travel overseas for two weeks following removal of polyps because bleeding can happen at any time up to two weeks later.
- A perforation (tear in the bowel). The risk of perforation is less than one in 1000. If a significant bleed or perforation were to happen, further treatment may be required such as a blood transfusion or surgery.
- Reaction to medication for example, sedation and painkillers.
- Missed pathology. Small polyps may be missed during examination.
What preparation will I need for my colonoscopy?
Your bowel must be completely empty of waste material (faeces) for the endoscopist to have a clear view.
The procedure may have to be repeated at a later date if your bowel is not empty.
Preparation instructions
|
Before your colonoscopy
|
It is important that you follow the dietary and medication instructions provided in the information leaflet. See enclosed leaflet. |
|
Day of colonoscopy
|
Unless you are told otherwise, please stop drinking clear fluids TWO HOURS before your appointment at the hospital. |
|
What should I bring on the day?
|
· If you are diabetic please bring your insulin or tablets. · Your prescription medication. · Your reading glasses so that you can read the consent form. · You are welcome to bring your own dressing gown and slippers. |
|
When you arrive Only one escort/relative will be able to accompany you due to limited space. If you need someone to support you, please call the unit to arrange. |
Please report to the Endoscopy Reception. You will be greeted by a nurse and then: · You will be asked several questions about your health and current medication. · Your blood pressure and pulse will be taken. · You may be asked to sign a consent form. · You will be asked to undress and change in to a theatre gown or if you have brought them, your own dressing gown and slippers. This will be a private single sex area. · A cannula (small needle) will be inserted so intravenous medication can be given. · Please talk to us about any worries or concerns that you may have. |
What about my medication?
- If you are taking any blood thinning medication for example, Warfarin, Clopidogrel, Apixiban, Rivaroxaban,etc., please contact the Endoscopy Unit by calling 01625 661044 or 01625 663333.
- There is no need to stop low dose aspirin, for example, 75mg/day.
- If you are diabetic, please contact the diabetic nurse specialist for advice by calling 01625 661083.
- If you take Iron tablets, please stop them five days before the test.
- If you have a stoma, please contact your specialist nurse for advice.
- If you have any other concerns about your medication, please seek advice from your GP.
Your colonoscopy procedure
The procedure will take place in the Endoscopy Procedure Room.
- You will be kept as comfortable as possible.
- You will need to lie on your left side.
- A nurse will stay with you throughout the procedure.
- Each stage of the procedure will be explained to you as it happens.
- Your oxygen levels and pulse will be monitored as well as your level of comfort.
- You may be given oxygen during the test, through little prongs that fit just inside your nostrils.
Procedure options
- ‘Gas and air’ (entonox). Some patients prefer this as they want to try to have the procedure carried out without any sedation. This can sometimes make them feel more comfortable and relaxed and wears off in half an hour.
- Sedative and painkiller. This method will help you to relax but it is not a general anaesthetic. This is given through a small needle placed in a vein on the back of your hand.
During your procedure
- The endoscopist will carefully pass the colonoscope through your bottom (anus) into your rectum and on into your colon.
- Some abdominal cramping and pressure is felt from the air which is introduced into your colon which is normal and will pass quickly.
- You may get the sensation of wanting to go to the toilet, but as the bowel is empty, there is no danger of this happening.
- You may feel you need to pass wind and, although this may be embarrassing, remember the staff do understand what is causing it.
- If you need to change position during the procedure, a nurse will help you.
- The nurse may need to press on your abdomen for a few moments during the procedure to help the colonoscope around awkward bends in your bowel. You will be warned before any pressure is applied.
- The endoscopist may take tissue samples (biopsies), photographs or a video of your bowel, even if it all looks normal.
- At the end of the examination, the colonoscope is removed quickly and easily.
- The procedure may take up to 45 minutes.
After your procedure
- You may feel bloated because air remains in your bowel. This will settle as you pass wind.
- Your blood pressure and pulse will be monitored.
- If you have been given intravenous sedation you will need to rest in the recovery area until you are fully awake.
- If you have used gas and air (entonox), you should be able to leave after 30 minutes as the sedative effects wear off quickly.
Going home
If you require sedation:
This impairs your reflexes and judgment so you do need to have responsible adult with you. Please note that your procedure will not be performed if you do not have an responsible adult with you.
For 24 hours after the procedure you must not:
- Drive
- Operate machinery.
- Drink alcohol.
- Sign legal documents.
If you have received entonox (gas and air):
- It wears off within 30 minutes and you should be able to drive home.
You will be given any written information that you need when you leave the hospital.
Your medication after the procedure
We will talk to you about your medication after the procedure and before you go home in case changes to your medication are needed.
When will I know the results?
You will be told about the results when you are ready to be discharged and provided with a copy of the colonoscopy report. A copy will also be sent to your GP or whoever referred you.
The consent form
You will find a consent form with this information. This gives the endoscopist a formal indication that you are agreeing to undergo the procedure as described. You keep a portion of the form as your record.
Please read the consent form and bring it with you to the appointment.
For further information, click here.
Concerns or questions
For further advice please contact the Endoscopy Unit between 8am and 6.30pm, Monday to Saturday.
Endoscopy Unit Tel: 01625 661044 or 01625 663333.
How to find us:
|
Macclesfield District General Hospital Victoria Road, Macclesfield, Cheshire, SK10 3BL Tel: 01625 421000 Endoscopy Unit is on the first floor. |
Please note car parking charges will apply.
What is a Gastroscopy?
A gastroscopy (or simple endoscopy) is a test which allows the endoscopist to look directly at the lining of the oesophagus (gullet), the stomach, and the first part of the small intestine (duodenum). In order to do this, a thin flexible tube called a gastroscope that transmits live video images to a TV monitor is passed through your mouth into your stomach.
Why am I having a Gastroscopy?
Your doctor wants to find out if there is a reason for the symptoms you are having so that they can suggest treatment. The endoscopist will get a clear internal view and find the cause of your symptoms. Importantly, this is the only test that allows biopsies to be taken for analysis.
Are there any alternatives to the test?
Yes, a barium swallow, barium meal or a computed tomographic colonography (virtual colonoscopy) which will show larger abnormalities of the mucosa (lining) however biopsies cannot be taken and polyps cannot be removed.
Are there any risks to the test?
The procedure is considered safe. Complications are rare but possible:
• If a biopsy is taken or a polyp removed it can lead to bleeding or a perforation (tear) of the bowel. Bleeding usually settles on its own. A perforation often requires surgery but the risk of this complication is small. The overall complication rate including perforation and bleeding is estimated to be less than one in 1,000 cases.
• Complications of sedation.
• Damage to teeth, crowns or bridges.
• Aspiration.
• You are likely to feel bloated and have some abdominal discomfort after the test.
• You may also have a mild sore throat.
Before admission
Do not eat or drink anything for six hours before the test. Please bring a list of your medication with you and your dressing gown and slippers.
What should I expect?
• On arrival, report to the reception desk in Endoscopy Unit. Your details will be checked and you will be asked to take a seat.
• A nurse will collect you and take a brief medical history from you, including a discussion of your current medication, discharge arrangements and the test itself.
Please inform the nurse of any allergies. Please ask questions if you have any.
• You may be asked to wait a short while until you have the test.
• A nurse or endoscopist will ask you to sign the consent form making sure you understand the test.
• You will be asked to change into a theatre gown and remove your underwear.
• You will be given an enema, which is inserted into the back passage. The large bowel, which normally contains faeces, must be clean to ensure safe, clear views. You will have a private room with its own toilet facilities.
• The ward is a single sex area.
Is the procedure painful?
The procedure can be uncomfortable so you will be offered Entonox which is a short acting pain relief in the form of gas you breathe in. This does not remain in your system so you would not need any special aftercare requirements. Sedation is also available which is given through a plastic tube (cannula) inserted into the back of your hand or arm. This will make you more comfortable but it does not put you to sleep, however you may forget the procedure afterwards, and there are special aftercare requirements for 24 hours after the procedure.
During the gastroscopy you may experience some retching as the tube touches the back of your throat. You may feel bloated and burp because air is put into your stomach to ensure good views. The test usually lasts around 15 minutes. These feelings are not pleasant but do not last long.
There are two ways you can have the Gastroscopy:
1. You can have local anaesthetic spray to the back of the throat which numbs the area and makes it easier to the pass the tube. It also reduces retching.
2. You can have a mild sedative which will help you feel more relaxed about the test. It does not put you to sleep.
If you do not wish to have any of these options, please inform the nurse.
During the test
• You will be taken into the procedure room. In the room will be the Endoscopist and two nurses who will stay with you during the test
• You will normally be given Entonox or a sedative injection unless you have requested otherwise.
• You will be made comfortable on your left side with your knees bent
• A pad will be placed under your chin and one under your bottom.
• A plastic mouth guard will be placed gently in your mouth.
• The endoscope will be passed across the top of your tongue to the back of your throat. Try to breathe steadily and remain calm.
• It will then be passed down the gullet, into the stomach and the small intestine.
You may feel bloated as air is used to inflate your stomach to get good views.
• Biopsies can be taken and this is painless.
• Photographs may be taken of normal and abnormal mucosa.
• If you get a lot of saliva in your mouth, the nurse will clear it using a suction tube.
• The endoscope is removed slowly taking some air out at the same time.
• The mouth guard will be removed and a tissue provided to wipe your mouth.
• The trolley you are lying on will be turned around.
• The Endoscopist will lubricate your back passage with a gloved finger and lubricating jelly.
• They will then pass the instrument into your back passage and manoeuvre it carefully around the bowel
• Biopsies can be taken or polyps removed.
• Photographs may be taken of normal and abnormal mucosa
• You may be asked to change positions and the nurses will help you do this
• The nurse may press on your abdomen to assist the manoeuvring of the
instrument
• The endoscope is removed slowly to ensure good views
• You will be covered and made comfortable
• You will be taken out to the ward area to recover.
When can I go home?
If you have had Entonox and/or throat spray then you would be allowed to leave the department when the effects have worn off normally no longer than 30 minutes. If you have had sedation then you will need to rest in the department for as long as necessary.
We will only discharge you when you are safe to go home and you feel happy to do so. You need to be collected from the unit by a responsible adult who will stay with you overnight.
If you have had sedation: FOR 24 HOURS, YOU MUST NOT:
• Drive
• Operate machinery
• Drink alcohol
• Sign legal documents
How will I feel afterwards?
• Your throat may feel sore but will settle without treatment.
• You may feel bloated because air remains in your bowel; it will settle as you pass wind
• If you have been sedated, you may feel tired and lethargic for the next 24 hours so you should rest
• You should be able to eat and drink as normal
When will I know the results?
When you are fully awake, you will be told about the test and anything that has been done. We prefer a family member or friend to be present as you may forget what you have been told because of the medication you have had. If you object to a family member being present, please inform the nurses. You will be given a discharge leaflet which includes aftercare, useful telephone numbers and information about your test. The hospital consultant responsible for your procedure will receive any biopsy results and will write to you or see you in Outpatients. A copy of the report will also be sent to your GP.
The consent form
You will find a consent form with this information. This gives the endoscopist a formal indication that you are agreeing to undergo the procedure as described. You keep a portion of the form as your record. Please read the consent form and bring it with you to the appointment.
For further information, click here.
What if I decide not to have the test?
If you read this information and decided not to go ahead with the test, please let us know by calling the Booking Centre on 01625 663333. You should also discuss your decision with your GP or hospital consultant.
What is a Flexible Sigmoidoscopy?
A flexible sigmoidoscopy is a test which allows the endoscopist to look directly at the lining of the left side of the large bowel (colon). This is done using an endoscope which has a thin flexible tube that transmits live video images to a TV monitor. This is passed into your anus (back passage) and around your bowel.
The test allows the endoscopist to painlessly take tiny pieces of tissue (biopsies) for analysis to assess the lining of the bowel. If a polyp (an overgrowth of tissue) is found this can often be removed painlessly during the procedure and again sent for analysis.
Why am I having a Flexible Sigmoidoscopy?
Your doctor wants to find out if there is a reason for the symptoms you are having so that he can suggest treatment. The endoscopist will get a clear internal view and find the cause of your symptoms. Importantly, this is the only test that allows biopsies or polyps to be taken for analysis.
Are there any alternatives to the test?
Yes, a computed tomographic colonography (virtual colonoscopy) which will show larger abnormalities of the mucosa (lining) however biopsies cannot be taken and polyps cannot be removed.
Are there any risks to the test?
The procedure is considered safe. Complications are rare but possible:
• If a biopsy is taken or a polyp removed it can lead to bleeding or a perforation (tear) of the bowel. Bleeding usually settles on its own. A perforation often requires surgery but the risk of this complication is small. The overall complication rate including perforation and bleeding is estimated to be less than one in 1,000 cases.
• Complications of sedation
• You are likely to feel bloated and have some abdominal discomfort after the test.
Before admission
Please refrain from having any food for two hours before this appointment. Please bring a list of your medication with you.
What should I expect?
• On arrival, report to the reception desk in Endoscopy Unit. Your details will be checked and you will be asked to take a seat.
• A nurse will collect you and take a brief medical history from you, including a discussion of your current medication, discharge arrangements and the test itself.
Please inform the nurse of any allergies. Please ask questions if you have any.
• You may be asked to wait a short while until you have the test.
• A nurse or endoscopist will ask you to sign the consent form making sure you understand the test.
• You will be asked to change into a theatre gown and remove your underwear.
• You will be given an enema, which is inserted into the back passage. The large bowel, which normally contains faeces, must be clean to ensure safe, clear views. You will have a private room with its own toilet facilities.
• The ward is a single sex area.
Is the procedure painful?
The procedure can be uncomfortable so you will be offered Entonox which is a short acting pain relief in the form of gas you breathe in. This does not remain in your system so you would not need any special aftercare requirements if you choose this option. Sedation is also available which is given through a plastic tube (cannula) inserted into the back of your hand or arm. This will make you more comfortable but it does not put you to sleep, however you may forget the procedure afterwards, and there are special aftercare requirements for 24 hours after the procedure.
If you do not wish to have any of these options, please inform the nurse
During the test
• You will be taken into the procedure room. In the room will be the endoscopist and two nurses who will stay with you during the test
• You will normally be given Entonox or a sedative injection unless you have requested otherwise.
• You will be made comfortable on your left side with your knees bent
• A pad will be placed under your bottom
• The endoscopist will lubricate your back passage with a gloved finger and lubricating jelly.
• They will then pass the instrument into your back passage and manoeuvre it carefully around the bowel
• Biopsies can be taken or polyps removed.
• Photographs may be taken of normal and abnormal mucosa
• You may be asked to change positions and the nurses will help you do this
• The nurse may press on your abdomen to assist the manoeuvring of the
instrument
• The endoscope is removed slowly to ensure good views
• You will be covered and made comfortable
• You will be taken out to the ward area to recover.
When can I go home?
If you have had Entonox then you would be allowed to leave the department when the effects have worn off normally no longer than 30 minutes. If you had sedation then you will need to rest in the department for as long as necessary. We will only discharge you when you are safe to go home and you feel happy to do so. You need to be collected from the unit by a responsible adult who will stay with you overnight.
If you have had sedation: FOR 24 HOURS, YOU MUST NOT:
• Drive
• Operate machinery
• Drink alcohol
• Sign legal documents
How will I feel afterwards?
• You may feel bloated because air remains in your bowel; it will settle as you pass wind
• If you have been sedated, you may feel tired and lethargic for the next 24 hours so you should rest
• You should be able to eat and drink as normal
When will I know the results?
You will be told what has been seen and done after the test. If you have been sedated, when you are fully awake, you will be told about the test and anything that has been done. We prefer a family member or friend to be present as you may forget what you have been told because of the medication you have had. If you object to a family member being present, please inform the nurses. You will be given a discharge leaflet which includes aftercare, useful telephone numbers and information about your test.
The hospital consultant responsible for your procedure will receive any biopsy results and will write to you or see you in Outpatients. A copy of the report will also be sent to your GP.
The consent form
You will find a consent form with this information. This gives the Endoscopist a formal indication that you are agreeing to undergo the procedure as described. You keep a portion of the form as your record.
Please read the consent form and bring it with you to the appointment.
For further information, click here.
What if I decide not to have the test?
If you read this information and decided not to go ahead with the test, please let us know by calling the Booking Centre on 01625 663333. You should also discuss your decision with your GP or hospital consultant.
What is a Gastroscopy?
A gastroscopy (or simple endoscopy) is a test which allows the endoscopist to look directly at the lining of the oesophagus (gullet), the stomach, and the first part of the small intestine (duodenum). In order to do this, a thin flexible tube called a gastroscope that transmits live video images to a TV monitor is passed through your mouth into your stomach.
Why am I having a Gastroscopy?
Your doctor wants to find out if there is a reason for the symptoms you are having so that he can suggest treatment. The endoscopist will get a clear internal view and find the cause of your symptoms. Importantly, this is the only test that allows biopsies to be taken for analysis.
What is a Colonoscopy?
A colonoscopy is a test which allows the endoscopist to look directly at the lining of the large bowel (colon). This is done using an endoscope which has a thin flexible tube that transmits live video images to a TV monitor. This is passed into your anus (back passage) and around your bowel.
The test allows the endoscopist to painlessly take tiny pieces of tissue (biopsies) for analysis to assess the lining of the bowel.
If a polyp (an overgrowth of tissue) is found this can often be removed painlessly during the procedure and again sent for analysis.
Why am I having a Colonoscopy?
Your doctor wants to find out if there is a reason for the symptoms you are having so that he can suggest treatment. The endoscopist will get a clear internal view and find the cause of your symptoms. Importantly, this is the only test that allows biopsies or polyps to be taken for analysis.
Are there any alternatives to the test?
Yes, a barium swallow, barium meal or a computed tomographic colonography (virtual colonoscopy) which will show larger abnormalities of the mucosa (lining) however biopsies cannot be taken and polyps cannot be removed.
Are there any risks to the test?
The procedure is considered safe. Complications are rare but possible:
• If a biopsy is taken or a polyp removed it can lead to bleeding or a perforation (tear) of the bowel. Bleeding usually settles on its own. A perforation often requires surgery but the risk of this complication is small. The overall complication rate including perforation and bleeding is estimated to be less than one in 1,000 cases.
• Complications of sedation.
• Damage to teeth, crowns or bridges.
• Aspiration.
• You are likely to feel bloated and have some abdominal discomfort after the test.
• You may also have a mild sore throat.
Before admission
Bowel preparation is included with this letter together with specific diet instructions for you to follow. It is essential that you follow these instructions exactly as the bowel needs to be clear for the test to be successful. Do not drink anything for two hours before the test. Please bring a list of your medication with you and your dressing gown and slippers.
What should I expect?
• On arrival, report to the reception desk in Endoscopy Unit. Your details will be checked and you will be asked to take a seat.
• A nurse will collect you and take a brief medical history from you, including a discussion of your current medication, discharge arrangements and the test itself. Please inform the nurse of any allergies. Please ask questions if you have any.
• You may be asked to wait a short while until you have the test.
• A nurse or endoscopist will ask you to sign the consent form making sure you understand the test.
• You will be asked to change into a theatre gown with your dressing gown and slippers on. Please remove your underwear.
• The ward is a single sex area.
Is the procedure painful?
The procedure can be uncomfortable so you will be offered Entonox which is a short acting pain relief in the form of gas you breathe in. This does not remain in your system so you would not need any special aftercare requirements if you choose this option or you will be offered a sedative and a painkilling injection which is given through a plastic tube (cannula) inserted into the back of your hand or arm. This will make you more
comfortable but it does not put you to sleep, however you may forget the procedure afterwards, and there are special aftercare requirements for 24 hours after the procedure. The colonoscopy makes you feel bloated and as if you need to go to the toilet. These sensations settle after the tests. During the gastroscopy you may experience some retching as the tube touches the back of your throat. You may feel bloated and burp because air is put into your stomach to ensure good views. The test usually lasts between five and 15 minutes. These feelings are not pleasant but do not last long.
There are two ways you can have the Gastroscopy:
1. You can have local anaesthetic spray to the back of the throat which numbs the area and makes it easier to the pass the tube. It also reduces retching.
2. You can have a mild sedative which will help you feel more relaxed about the test.
It does not put you to sleep. If you do not wish to have any of these options, please inform the nurse.
During the test
• You will be taken into the procedure room. In the room will be the endoscopist and two nurses who will stay with you during the test
• You will normally be given Entonox or a sedative injection unless you have requested otherwise.
• You will be made comfortable on your left side with your knees bent
• A pad will be placed under your chin and one under your bottom.
• A plastic mouth guard will be placed gently in your mouth.
• The endoscope will be passed across the top of your tongue to the back of your throat. Try to breathe steadily and remain calm.
• It will then be passed down the gullet, into the stomach and the small intestine.You may feel bloated as air is used to inflate your stomach to get good views.
• Biopsies can be taken and this is painless.
• Photographs may be taken of normal and abnormal mucosa.
• If you get a lot of saliva in your mouth, the nurse will clear it using a suction tube.
• The endoscope is removed slowly taking some air out at the same time.
• The mouth guard will be removed and a tissue provided to wipe your mouth.
• The trolley you are lying on will be turned around.
• The Endoscopist will lubricate your back passage with a gloved finger and lubricating jelly.
• They will then pass the instrument into your back passage and manoeuvre it carefully around the bowel
• Biopsies can be taken or polyps removed.
• Photographs may be taken of normal and abnormal mucosa
• You may be asked to change positions and the nurses will help you do this
• The nurse may press on your abdomen to assist the manoeuvring of the
instrument
• The endoscope is removed slowly to ensure good views
• You will be covered and made comfortable
• You will be taken out to the ward area to recover.
When can I go home?
If you have had Entonox and/or throat spray then you would be allowed to leave the department when the effects have worn off normally no longer than 30 minutes. If you have had sedation then you will need to rest in the department for as long as necessary. We will only discharge you when you are safe to go home and you feel happy to do so. You need to be collected from the unit by a responsible adult who will stay with you overnight.
If you have had sedation: FOR 24 HOURS, YOU MUST NOT:
• Drive
• Operate machinery
• Drink alcohol
• Sign legal documents
How will I feel afterwards?
• Your throat may feel sore but will settle without treatment.
• You may feel bloated because air remains in your bowel; it will settle as you pass wind
• If you have been sedated, you may feel tired and lethargic for the next 24 hours so you should rest
• You should be able to eat and drink as normal
When will I know the results?
When you are fully awake, you will be told about the test and anything that has been done. We prefer a family member or friend to be present as you may forget what you have been told because of the medication you have had. If you object to a family member being present, please inform the nurses. You will be given a discharge leaflet which includes aftercare, useful telephone numbers and information about your test. The consultant responsible for your procedure will receive any biopsy results and will write to you or see you in Outpatients. A copy of the report will also be sent to your GP.
The consent form
You will find a consent form with this information. This gives the endoscopist a formal indication that you are agreeing to undergo the procedure as described. You keep a portion of the form as your record.
Please read the consent form and bring it with you to the appointment.
For further information, click here.
What if I decide not to have the test?
If you read this information and decided not to go ahead with the test, please let us know by calling the Booking Centre on 01625 663333. You should also discuss your decision with your GP or hospital consultant.
ERCP Procedure Information
All the information you need on the procedure can be found be clicking here.
Giving my consent (permission):
We want to involve you in decisions about your care and treatment. If you decide to go ahead, you will be asked to sign a consent form. This states that you agree to have the treatment and you understand what it involves. Please read the consent form and bring it with you to your appointment.
What if I decide not to have the test?
If you read this information and decided not to go ahead with the test, please ring the department, using the telephone number on your appointment letter, to let us know. You should also discuss your decision with your GP or hospital consultant.
Macclesfield District General Hospital
Investigative respiratory procedures are performed two days-a-week on Wednesday and Thursday in the afternoon at East Cheshire and include:
Diagnostic flexible bronchoscopy
This helps us to visualise the breathing passages of the lungs (called 'airways'). It is done to see inside the airways of your lungs, or to get samples of mucus or tissue from the lungs.
EBUS (Endobronchial Ultrasound) and transbronchial needle aspiration
This procedure allows us to visualise the breathing tubes (similar to a bronchoscopy) and take sampling from enlarged glands (lymph glands) within the chest. This is done by using the aid of an ultrasound scan which is present at the end of a telescope and taking samples from the glands which lie outside the normal breathing tubes (bronchi).
Pleural aspiration
This procedure involves passing a small needle through the chest wall to remove fluid from the space between the lung and the inside of the chest wall (the pleural space). This fluid is referred to as a pleural effusion. This procedure is done using numbing agent (local anaesthetic) under the guidance of ultrasound.
Medical thoracoscopy
This is an examination of the inside of chest cavity, the space between your lung and the inside of chest wall (the pleural space). This allows a detailed assessment of the pleural space using a camera, to look for any abnormalities specifically on the lining of the lung (pleura) to help diagnose the cause of the fluid. This procedure is done using numbing agent (local anaesthetic) and sedation under the guidance of ultrasound.
East Cheshire NHS Trust's Endoscopy Unit is a hub for the bowel cancer screening programme.
This programme is designed for asymptomatic patients.
For bowel cancer screening information, click here.
For general information: www.bowelcancer.uk, www.cancerresearchuk.org
After the treatment
Most patients receive a normal result, but about two percent receive a positive or abnormal result. Patients with a positive result will be invited to see a specialist nurse and may be referred for a colonoscopy, an examination of the lining of the large bowel (colon) using a tiny camera on the end of a flexible tube.
- About five in 10 people who have a colonoscopy will have a normal result.
- Four in 10 people who have a colonoscopy will be found to have a 'polyp'.
- About one in 10 people who have a colonoscopy will have cancer detected.
Clinics
Nurse-led clinics are run at Leighton Hospital, Middlewich Road, Crewe, part of Mid Cheshire Hospitals NHS Foundation Trust.
Bowel Cancer Screening Team
The bowel cancer screening team are working hard to increase awareness and eventually improve outcomes for patients with bowel cancer in East Cheshire.
The NHS Bowel Cancer Screening Programme (BCSP) offers screening every two years to all men and women. Its aim is to identify people who appear healthy but are at an increased risk of developing bowel cancer. Over the next four years or so the screening programme is 'age expanding'; it will include people aged 50-58 and our screening centre has now commenced with screening for 56-year-olds. Anyone above the age of 74 can opt into the programme by telephoning the free phone hub on 0800 707 60 60. From April 2022, 58-year-olds will be invited. People aged 60-74 will continue to be invited when they are due to be screened.
Age Expansion is very exciting for the screening programmes across England.
The team are regularly out in the local area speaking to the public about the importance of bowel cancer screening and explaining the importance of early detection and diagnosis. Bowel cancer affects around 42,000 people in the UK every year and is the second most common cause of cancer death, with one in 20 people developing bowel cancer during their lifetime. Each year around 16,000 people die from bowel cancer. The work that the team are carrying out is aimed at improving the diagnosis and eventual prognosis for patients with bowel cancer.
The service has received excellent feedback from patients and highlights the importance of patient engagement to help improve and develop the programme.
Further information and support
The Macmillan Cancer Support and Information Centre
At the centre, staff will:
- Listen to how cancer is affecting your life
- Provide a wide range of free booklets and other written information
- Put you in touch with other sources of support such as local counselling services, benefits advisers and support groups
The centre is located at The Christie at Macclesfield, Macclesfield District Hospital, Macclesfield, SK10 3BL.
Opening hours are Monday to Thursday between 8.30am and 5pm and Friday between 8.30am and 4pm.
We are pleased to offer our highly-anticipated service for colon capsule endoscopy (CCE). This may be used as an alternative to colonoscopy in some cases and will be discussed with you by your consultant.
Colon capsule endoscopy is a less invasive procedure, where a special capsule containing a small camera is swallowed, allowing images of the bowel to be recorded as it travels through the gut.
The images are recorded onto a monitor worn by the patient.
The capsule is excreted and simply flushed away and the recorder returned to the hospital for analysis of the images.
Bowel Preparation Advice
Deprending on which bowel prep your clinician has chosen to prescribe for you, please see according advice linked below:
Taking Moviprep oral bowel cleansing agents safely and effectively for colonoscopy/flexible sigmoidoscopy - click here
Plenvu advice - morning appointment - click here
Plenvu advice - afternoon appointment - click here
Patient Feedback
We very often receive lovely comments from our patients following their care at East Cheshire NHS Trust.
Here is just a snapshot of the type of feedback we get. We hope that reading it will help to bolster your confidence in the knowledge and skill of our amazing team:
"The whole experience was first class. I was a little apprehensive but was made to feel completely at ease. Can't praise the staff highly enough."
"All the medical staff were efficient and helpful which made my procedure more comfortable than expected."
"You could not have given a better service, all staff was very polite ,friendly and helpful I got my appointment by telephone and and very pleased it was so quick."
"I was a little nervous but the staff straight away put me at ease and everything went smoothly. Thanks again."
"Fantastic treatment, professional friendly staff. Made you feel at ease, could not do anymore to help, top people. Thanks."
"I felt the treatment by medical staff seemed given with great sensitivity to patients needs... and the young nurses on the ward were very helpful in making sure you felt at ease."
"As always, the endoscopy staff were amazing, very attentive, caring and thorough in their care, before, during and after the procedure. I left fully informed and had an enjoyable experience considering the not so pleasant procedure. I have to have colonoscopies regularly and the standards of care in this dept remain consistently high. Thanks."
"Pleasant polite friendly helpful staff. Informed and explained thoroughly. Care was magnificent. Thank you."
"Lovely staff from reception, admitting staff nurse, team undertaking exam and post op recovery. All questions answered honestly and respectively. Put me at ease and made a worrying exam less so!"
"The staff on the Endoscopy Unit made me feel welcome and secure... A colonoscopy is not the most enjoyable experience but I was treated with professionalism, curtesy, kindness and concern for my well being... Well done all."
NHS Choices
You can share your experience of our services on NHS Choices. NHS Choices is a national website similar to the trip advisor you see on holiday and hotel websites.
Visit the NHS Choices website and type in which hospital you visited.
Your comments can also help us to improve things for future patients.
1. What is a low fibre diet?
Low fibre diet consists of:
White meat, skinless chicken, grilled or poached fish.
White bread, rice, pasta, boiled or mashed potatoes.
Cheese, eggs, tofu.
Shredless marmalade or jam no seeds.
Butter, margarine.
Natural plain yogurt.
Ice cream, custard.
Clear soup, black tea or coffee without milk, diluted cordial NOT BLACKCURRANT, herbal tea, water,
All the above of the above are on the Plenvu leaflet.
2. When should I take my first dose of Plenvu?
If you have a morning appointment you take your first dose of Plenvu the day before at 17.00 and 20.00.
If you have an afternoon appointment take your first dose of Plenvu at 19.00 the day before and 06.00 the morning of the procedure.
3. What does ETU stand for?
ETU stands for Endoscopy and Treatment Unit.
4. Where is the ETU at East Cheshire NHS Trust?
ETU is on the first floor of the main Macclesfield hospital site and is open Monday to Friday from 8am-6.30pm.
5. How long does a procedure take?
A gastroscopy can take up 20 minutes.
A flexible sigmoidoscopy can take up to 30 minutes.
A colonoscopy can take up to one hour.
This is an estimation of time dependant on whether the procedures are diagnostic or treatment is required in which case the time could be longer.
6. How long should someone stay with me after sedation?
If you choose to have sedation you must have someone to drop you and pick you up and stay overnight with you because sedation can stay in your system for up to 24 hours and impair your judgment.
More Patient Information
Abdominal Pain - click here
Acid Reflux and Oesophagitis (Heartburn) - click here
Bowel Polyps (Colonic Polyps) - click here
Fibre and Fibre Supplements - click here
Hiatus Hernia - click here
Irritable Bowel Syndrome (IBS) - click here
Piles (Haemorrhoids) - click here
Endoscopy and Treatment Unit Patient User Group
Do you want to be more involved in shaping the service you use?
The Endoscopy & Treatment Unit at Macclesfield Hospital is running a patient user group
By joining you will:
- Provide feedback on your experience
- Inform us what works and how we can improve the service we deliver to our patients
- Help spread good practice
- Share your experiences with other patients
- Contribute ideas and shape service developments
We are keen for our patient's to be actively involved in contributing constructive ideas to the future planning of the service
If you are interested in joining us, please let a member of the reception or nursing team know and they will take your details. Alternatively, you can email the team at ecn-tr.endoscopy@nhs.net. Somebody will be in touch with you nearer the time with further information.
Macclesfield District General Hospital
For information on how to get to the hospital and location map, click here.
For parking information, including drop-offs and pick-ups, click here.
Found a problem? Report it and help us to improve our website
